|
Anatomy and Function
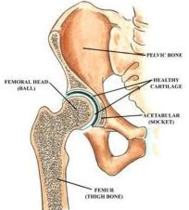
- The hip is a ball and socket joint comprised of the acetabulum and the proximal aspect of the femur ending 5 cm distal to the lesser tubercle.
- There is a strong fibrous capsule that surrounds the joint on all sides. The capsule extends from the acetabulum proximally to the femoral neck posteriorly and the intertrochanteric line anteriorly.
- The function of the hip is to distribute weight to the lower extremities and allow movement including flexion, extension, internal and external rotation, abduction and adduction.
- Vascular supply of the proximal femur is tenuous. It has essentially three main sources: the epiphyseal arteries, the metaphyseal arteries, and the foveal artery of the ligament teres.
- Disruption of the femoral neck or joint capsule can disrupt flow to the femoral head resulting in avascular necrosis.
- Sensory innervation to the hip joint is through the femoral, obturator, sciatic and superior gluteal nerves.
Trauma
Hip Dislocation
- In adults, significant force is required to dislocate the hip.
- Motor vehicle accidents are a common cause of hip dislocations, and they are often associated with multisystem trauma.
- Children and individuals with prosthesis require minimum force to cause hip dislocation.
- Hips can dislocate anterior, posterior or central.
- Posterior dislocation is most common, followed by anterior and central dislocations.
- It is important to look for associated hip fractures in both the high speed motor vehicle patient as well as the osteoporotic older patient.
- Children can have associated slipped capital femoral epiphysis.
- Hips should be relocated no later than 12 h after the event.
- Delay in reduction places the patient at increase risk for femoral head necrosis.
Presentation and Complications
Anterior Dislocation
- Anterior dislocations commonly occur after a fall or injury where the femur is abducted suddenly.
- There are three types of anterior dislocations including superior iliac, superior pubic and inferior (obturator) depending on the anatomic position of the femoral head after dislocation.
- Superior iliac dislocation presents with the hip extended and externally rotated.
- Superior pubic dislocation presents with the hips flexed, abducted, externally rotated.
- Inferior dislocation presents markedly flexed, abducted and externally rotated. Complications of anterior dislocation include disruption of the femoral artery, nerve and vein, postrraumatic arthritis and pulmonary embolism.
Posterior Dislocation
- Posterior dislocations are commonly caused in motor vehicle accidents when the knees hit the dashboard.
- The affected hip presents shortened, flexed, and internally rotated.
- Complications include sciatic nerve injury, femoral head necrosis, posttraumatic arthritis, and pulmonary embolism.
Central Dislocation
- Central dislocation refers to the disruption of the acetabulum with the femoral head displaced into the pelvis.
- Surgical reduction is required.
Management and Treatment
Initial Assessment
- As with all trauma, airway, breathing, and circulation should first be assessed and managed.
- Assess the patient�s neurologic and vascular status of the affected extremity.
- In anterior dislocations, check the patient�s femoral, popliteal, and pedal pulses. Diminished pulses, swelling of the thigh, weakness of the quadriceps, diminished patellar reflex, or decreased sensation of the anteromedial thigh should alert the ED physician to femoral nerve or vascular injury.
- If a posterior dislocation is suspected, check for sciatic nerve impairment: assess the posterolateral leg and sole of the foot for sensation, and flexors of the knee for strength.
- Careful documentation should be noted before and after reduction.
- Early analgesia or local anesthesia (in the elderly or unstable patient) is recommended.
Radiography
- Plain radiographs in two views are necessary to evaluate the dislocated hip.
- The AP view and the lateral view are the most common.
- Films must be evaluated for occult fractures of the acetabulum, femoral head, femoral neck and femoral shaft prior to reduction.
- Additional views including the judet, 15 degree oblique and the cross-table axiolateral view as well as CT may be needed to adequately assess these areas.
- To distinguish between anterior and posterior dislocation, assess the femoral head size and the position of the lesser trochanter.
- In anterior dislocations the femoral head appears larger than the opposite side and the lesser trochanter is easily visualized.
- In posterior dislocations the femoral head appears smaller and the lesser trochanter will be superimposed on the femoral shaft.
Reduction
- If a dislocation is associated with a fracture, reduction is controversial depending on the location and type of fracture.
- Orthopedic consultation is recommended.
- If no fracture is present, then conscious sedation and primary closed reduction is the treatment of choice:
- Anterior dislocation is best reduced with the Allis maneuver. The patient is place supine, the pelvis is stabilized at the ASIS, and gentle traction is applied in the line of the deformity. The hip is slowly flexed to 90 degrees then slowly internally and externally rotated.
- Posterior dislocation is best reduced with the Stimson maneuver. The patient is placed prone, and the pelvis is stabilized at the sacrum. The limb is allowed to hang over the table and positioned in flexion at the hip, knee, and ankle at 90 degrees.
- Gentle downward traction is placed just distal to the knee.
- If reduction is not obtained easily then orthopedic consult and open reduction must be considered.
- After all reductions, post-reduction films and neurovascular assessment is critical.
Disposition
- All hip dislocations require orthopedic consult. Most hip dislocations require admission.
Hip Fracture
Epidemiology
- Hip fractures account for over 250,000 hospital visits annually in the US. They are associated with a high morbidity and mortality.
- One-year mortality rates are as high as 14-36% in the elderly. (N Engl J Med 334:1519-25, 1996).
- The mechanism of injury is commonly minor trauma in the elderly compared to high energy trauma in the young adult.
- Fractures, dislocations, and fracture dislocations are an orthopedic emergency.
ManagementM
- Hip fractures have a broad spectrum of presentation.
- They may present with an ambulatory elderly person complaining of groin, hip, thigh, or knee pain to the hypotensive multisystem penetrating or blunt trauma patient.
- Management is tailored to the presentation.
Prehospital Care
- The ABCs should be assessed and treated initially.
- After stabilization, a brief neurovascular exam of the extremity should be performed.
- Open wounds should be dressed with a sterile dressing. Bleeding should be stopped with direct pressure.
- The patient should be splinted and placed in a position of comfort.
- Traction devices such as a Hare splint may be placed as it can reduce pain and can tamponade further blood loss.
- Contraindications to traction include open fractures, suspected sciatic nerve injury, fracture of the ipsilateral pelvis or lower extremity, and fractures near the knee.
ABCs
- Patients� airway, breathing, and circulation must be stabilized initially.
- Once assessed and treated, the hip fracture should be evaluated during the secondary survey.
Physical Exam
- Signs and symptoms of hip fracture include tenderness, ecchymosis, deformity, and shortening.
- Examine the wound and determine if it is open or closed.
- Evaluate neurologic and vascular status. Check the deep tedon reflexes, sensation, and pedal pulses.
- If vascular injury is suspected, compare the blood pressures of the injured and noninjured extremity.
- Pay close attention to sciatic nerve injury (see hip dislocation).
- Evaluate the entire extremity for associated injuries (femoral shaft, knee, tibia and fibula).
Radiography
- Plain films should be performed as soon as possible.
- Splints should be removed to obtain adequate films.
- AP pelvis and a lateral hip film are standard.
- If necessary, an oblique hip with the femur internally rotated at 15-20 degrees will enhance visualization of the femoral neck.
- If a fracture is not identified on plain films but is highly suspected, a CT, bone scan or preferably a MRI must be performed to rule out fracture.
Treatment
- Adequate analgesia is pertinent.
- Opioid analgesia is recommended.
- In the unstable patient where narcotics use is not acceptable, a femoral nerve block can be used to reduce pain.
- Patients with open fractures should be started on antibiotics immediately.
- For a clean open wound less than 1 cm, a first-generation cephalosporin should be started.
- For wounds that appear contaminated or are >1 cm, antibiotics with Gram-negative and Gram-positive coverage should be used.
- Tetanus prophylaxis should be given.
- All fractures require orthopedic consultation and admission.
Classification and Associated Complications
There are multiple classification systems for hip fractures. However, hip fractures can easily be described by location. Presentation, treatment, and complications are different with each fracture.
- Intracapsular
- Femoral head
- Femoral head fractures are most commonly associated with dislocations.
- The incidence of femoral head fractures in anterior dislocations is between 22-77% while the incidence of fractures in posterior dislocations is between 10-16%.
- It is imperative to obtain post-reduction AP pelvis films and assess for femoral head fractures.
- Fractures can be very subtle, and if suspected a CT or MRI should be obtained. Avascular necrosis and post-traumatic arthritis are the most common complications.
- Femoral neck
- Femoral neck fractures can be nondisplaced (Garden Type I-II) or displaced (Garden Type III-IV).
- Femoral neck fractures occur most commonly in low energy fractures in the elderly.
- In younger patients they may result from multisystem trauma.
- Young patients will have an assosciated femoral shaft fracture 20% of the time, and the femoral neck fracture can be overlooked.
- A high index of suspicion should be maintained and appropriate imaging modalities used.
- Nondisplaced fractures or those with other injuries may not be visualized, and MRI or bone scanning is necessary.
- Avascular necrosis is the most common complication of femoral neck fractures.
- The incidence is higher in displaced fractures and increases with delay of definitive treatment.
- The remaining complications are due to prolonged immobilization and nonunion.
- Extracapsular
- Trochanteric
- Trochanteric fractures are uncommon and usually seen in young or old patients after a direct fall.
- Trochanteric fractures are either displaced or nondisplaced fractures of the lesser or greater trochanter.
- Fractures of the lesser trochanter are commonly avulsion fractures.
- Nondisplaced fractures can be treated with bed rest and analgesia.
- In the young patient, displaced greater trochanteric fractures >1cm or lesser trochanteric fractures >2 cm require internal fixation.
- Complications include associated muscle funtion loss, but generally outcome and function are good.
- Intertrochanteric
- The classic intertochanteric fracture consists of the fracture line between the greater and lesser trochanter.
- It is seen most commonly in the elderly after falls.
- Intertrochanteric fractures can be classified as stable or unstable.
- Unstable fractures are those that are displaced, comminuted or with multiple fracture lines.
- Definitve treatment is almost always open reduction and internal fixation.
- Moribidity is high-49% of patients sustaining intertrochanteric fractures are unable to regain their original ability to ambulate (J Bone Joint Surg 60A:930, 1978).
- Mortality is associated with complications of immobilization including pulmonary embolism, pneumonia, UTIs, decubitus ulcers etc.
- Subtrochanteric
- The subtrochanteric region is the area between the lesser trochanter to a point 5 cm distally.
- In the elderly, fractures commonly occur secondary to low energy trauma and poor bone quality.
- In the young, the fracture is secondary to high energy trauma.
- Pathologic fractures are common at this site.
- Definitive care is controversial but orthopedic consultation is always required.
- Traction splinting is recommended.
- Subtrochanteric fracture complications include significant blood loss, associated injuries of high energy trauma, and nonunion.
Disposition
- All fractures require orthopedic consultation and admission.
- Open reduction and internal fixation versus arthroplasty is dependent on the type of fracture, the age and condition of the patient, and the condition of the bone.
|