Human Immunodeficiency Virus
|
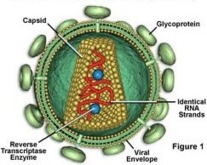 The appearance of the human immunodeficiency virus (HIV) approximately two
decades ago has changed the face of medicine. HIV infected patients are at risk for
opportunistic infections and many require additional prophylactic antimicrobial
therapy. Each year numerous developments in the management of HIV infection, primarily new medications, are introduced. In 1986 zidovudine was the first antiretroviral approved for the treatment of HIV infection. Today 16 antiretroviral drugs are currently available. Patients infected with HIV are treated with complex regimens of antiretroviral "cocktails" including reverse transcriptase inhibitors, protease inhibitors, and nonnucleoside reverse transcriptase inhibitors. Each medication has numerous side effects, some of which are lethal. This chapter reviews the common problems faced by emergency physicians when treating HIV infected patients, opportunistic infections and reactions to highly active antiretroviral therapy (HAART).
The appearance of the human immunodeficiency virus (HIV) approximately two
decades ago has changed the face of medicine. HIV infected patients are at risk for
opportunistic infections and many require additional prophylactic antimicrobial
therapy. Each year numerous developments in the management of HIV infection, primarily new medications, are introduced. In 1986 zidovudine was the first antiretroviral approved for the treatment of HIV infection. Today 16 antiretroviral drugs are currently available. Patients infected with HIV are treated with complex regimens of antiretroviral "cocktails" including reverse transcriptase inhibitors, protease inhibitors, and nonnucleoside reverse transcriptase inhibitors. Each medication has numerous side effects, some of which are lethal. This chapter reviews the common problems faced by emergency physicians when treating HIV infected patients, opportunistic infections and reactions to highly active antiretroviral therapy (HAART).
Opportunistic Infections
- The precise opportunistic infection (OI) any given patient will develop depends upon
the level of immunosuppression and the types of exposures the patient experiences.
Pneumocystis carinii Pneumonia (PCP)
- P. carinii is an organism of low virulence in the immunocompetent host and is found
in the lungs of both humans and animals worldwide.
- PCP continues to be a common OI in North America and is a common presentation
in those newly diagnosed with HIV infection. Despite prophylaxis with trimethoprim/
sulfamethoxazole and the ensuing reduction in the incidence of PCP, this infection
remains a substantial cause of morbidity and mortality.
Clinical Presentation
- PCP is an interstitial pneumonia with an insidious onset of shortness of breath, dry
cough, and fever that develops over weeks to months, usually in HIV infected patients
with CD4 count <200.
- Tachypnea and tachycardia are common findings, and auscultation of the lungs reveals
crackles in approximately one-third of infected adults. Hypoxemia and an elevated
arterial-alveolar gradient may be noted and are reflections of the severity of disease.
- The chest radiograph classically shows bilateral diffuse interstitial infiltrates. Unilateral
infiltrates, cavities, pneumatoceles, lymphadenopathy, effusions and normal appearances
on chest radiograph are atypical, but do occur.
- Serum lactic dehydrogenase (LDH) may also be elevated but is nonspecific.
- P. carinii is rarely found in expectorated sputum but may be detected by inducing
sputum with inhaled saline. Fiberoptic bronchoscopy has the highest yield of >90%.
ED Management
- Many patients with mild to moderate disease are treated empirically based on clinical
diagnosis.
- Trimethoprim/sulfamethoxazole remains the drug of choice and may be administered
either orally or intravenously. The dose is 15-20 mg/kg/day trimethoprim and 75-100
mg/kg/day sulfamethoxazole in 3 or 4 divided doses. Clindamycin (900 mg IV q 8 h)
plus primaquine (30 mg po q day) is an alternative therapy for patients who are allergic
to sulfa medications. Other alternatives include atovaqone (750 mg po BID), pentamidine
(4 mg/kg/d IV).
- Prednisone is indicated for patients who are hypoxic (pO2 < 70 mm Hg) and should be
administered 15-30 min before the antibiotics are given. The dose is 40 mg po BID
for 5 days, then 40 mg po q day for 5 days, and then 20 mg po q day for 11 days.
Toxoplasmosis
- Taxoplasma gondii is a coccidian parasite that infects animals and humans worldwide.
Infection in immunocompetent individuals is rarely of clinical significance, but in
immunocompromised patients infection commonly involves the brain, lungs, and eyes.
- Encephalitis is the most common presentation, and it may demonstrate a wide array
of clinical manifestations including altered mental status, weakness, sensory abnormalities,
meningismus, cerebellar signs, movement disorders, seizures, and neuropsychiatric
disturbances.
- Presumptive diagnosis is made by detecting multiple bilateral cerebral lesions on computer
tomography of the brain. The lesions are "ring-enhancing", or contrast enhancing
in up to 80% of patients. A single lesion may be seen with Toxoplasma encephalitis
in up to 40% of patients, but the suspicion for central nervous system (CNS)
lymphoma is elevated with this finding.
- These patients should be admitted and treated with oral pyramethamine, folinic acid
and either sulfadiazine or clindamycin for 2 wk.
- Maintenance therapy is required for life due to a relapse rate of 80%.
Cytomegalovirus (CMV)
- Retinitis is the most common manifestation of CMV disease and usually occurs when
the patient�s CD4 cell count is < 50 cells/mm3. CMV also causes esophagitis, enteritis,
colitis, and pneumonia.
- The symptoms of CMV retinitis are nonspecific and include floaters, flashing lights,
loss of visual field, or a vague sense of visual loss. Visual impairment caused by focal
necrotizing retinitis can rapidly progress to blindness.
- The presumptive diagnosis is made by observing white fluffy retinal infiltrates occurring
within areas of hemorrhage on fundoscopic exam.
- Treatment with intravenous gancyclovir or foscarnet is usually empiric due to the
invasive nature of obtaining retinal or vitreous material for examination.
Cryptococcus
- Cryptococcus neoformans is a ubiquitous encapsulated organism.
- Cryptococcus fungus causes subacute meningitis, as well as pneumonia and skin lesions,
in patients with T-cell defects. AIDS is the predisposing factor in approximately
90% of cases.
- The presenting symptoms of crytococcal meningitis are mild and nonspecific, such as
nausea, headache, dizziness, irritability, somnolence, or confusion. Cranial nerve dysfunction
and papilledema are noted in up to 20% and 30%, respectively. Seizures
occur late in the course of infection. Fever is not always present and neurologic examination
is often normal. Most patients have minimal or no nuchal rigidity.
- Diagnosis is made by identifying the yeast in the cerebrospinal fluid (CSF) with an
India ink preparation, by cryptococcal antigen detection, or by culture. Over 90% of
patients will test positive for serum cryptococcal antigen. The opening pressure of the
CSF during lumbar puncture is often elevated, and the CSF glucose is decreased.
Usually more than 20 white blood cells are noted. A normal CSF profile in the setting
of suspected cryptococcal meningitis mandates fungal culture of the CSF.
- Routine laboratory testing, i.e., CBC and sedimentation rate, are usually normal.
- The treatment of choice is intravenous amphotericin B (0.5 0.8 mg/kg/d IV) plus 5
FC (25 mg/kg po q 6 h) for 2 wk or until the patient is clinically stable is. Oral
fluconazole is required for lifelong suppressive therapy.
Suggested Reading
- USPHS/IDSA Prevention of Opportunistic Infections Working Group. 1999
- USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected
with Human Immunodeficiency Virus. Clin Infect Dis 2000; 30:S29-65.
| Table: Adverse reactions of nucleoside reverse transcriptase inhibitors |
|---|
Zidovudine (AZT, Retrovir)
headache
nausea
bone marrow suppression
myopathy |
Didanosine (ddI, Videx)
diarrhea
peripheral neuropathy
pancreatitis
elevation of ALT/AST |
Zalcitabine (ddC)
peripheral neuropathy
stomatitis
rash |
Stavudine (d4T,Zerit)
peripheral neuropathy
gastrointestinal upset
headache
elevated ALT/AST
| Lamivudine (3TC, Epivir)
nausea
headache
fatigue
insomnia
| Abacavir (Zigen)
hypersensitivity reaction
nausea/vomiting/ diarrhea
severe rash
fever |
| Warrants discontinuation of all antiretrovirals |
Highly Active Antiretroviral Therapy (HAART)
- The widespread use of combination therapy with multiple antiretroviral agents has
reduced the morbidity and mortality due to HIV infection. Death rates due to HIV
have declined as much as 65% in the United States. Despite these optimistic results,
only one-half of patients achieve maximal viral suppression. Many factors prevent
successful treatment including viral resistance, inadequate adsorption due to gastrointestinal
disease, lack of adherence to complex drug regimens, adverse drug effects, expense,
and coincident mental health and substance abuse problems.
- Emergency physicians should never discontinue HAART unless potentially lethal adverse
effects develop. If this situation occurs, then all antiretrovirals should be stopped
simultaneously to prevent the development of resistance.
- Many new antiretroviral agents are currently under development and emergency physicians
must continue to be vigilant and prepare for the recognition and management
of adverse effects.
Nucleoside Reverse Transcriptase Inhibitors
- The first class of antiretrovirals to be introduced was the nucleoside reverse transcriptase
inhibitors (NRTIs). There are currently six NRTI�s available and although their mechanism
of action is similar, adverse reactions for each agent are unique.
- Common symptoms include fever, rash, and gastrointestinal complaints. Over 85%
of cases began within the first 6 wk of therapy. A rare but deadly adverse reaction is
lactic acidosis with severe hepatomegaly. Other common adverse reactions are listed in
table.
- Adefovir dipiroxil is a novel nucleotide reverse transcriptase inhibitor. Renal toxicity is
the most important adverse effect and is seen in over one-third of patients. Adefovir
should be discontinued if renal function is impaired.
Nonnucleoside Reverse Transcriptase Inhibitors
- All NNRTIs are capable of causing a rash that may be mild and self-limited or severe and
capable of progressing to Stevens-Johnson syndrome. Mild rashes are treated with oral
antihistamines or topical steroid creams. Antiretrovirals may be continued and the patient
promptly reevaluated by their primary physician. However, if the rash is severe or
associated with fever, severe pruritis, ulcers, blisters, vomiting, diarrhea, mucosal involvement,
or muscle or joint pain, then all antiretrovirals must be discontinued.
- Common adverse reactions of the NNRTIs are listed in (Table 11.8).
| Table: Adverse reactions of non-nucleoside reverse transcriptase inhibitors |
|---|
Nevirapine (Viramune)
Stevens-Johnson syndrome
severe rash
fever
elevated ALT/AST
headache |
Delavirdine (Rescriptor)
severe rash
diarrhea
fatigue
headache |
Efavirenz (Sustiva)
CNS effects
severe rash
elevated ALT/ALT |
| Warrants discontinuation of all antiretrovirals |
| Table: Adverse effects of protease inhibitors |
|---|
Saquinovir (Invirase)
gastrointestinal symptoms
elevated ALT/AST |
Indinavir (Crixivan)
nephrolithiasis
hyperbilirubinemia
gastrointestinal symptom |
Ritonivir (Norvir)
gastrointestinal symptoms
headache
elevated ALT/AST
taste perversion |
Nelfinavir (Viracept)
diarrhea
nausea |
Amprenavir (Angenerase)
severe rash
nausea/vomiting
headache |
Lopinavir/ritonivir (Kaletra)
gastrointestinal symptoms
headache
weakness |
| Warrants discontinuation of all antiretrovirals |
Protease Inhibitors
- Adverse effects are common. Other complications include hyperlipidemia,
hyperglycemia, diabetes, and fat redistribution.
|