Chest CT
Trauma
Although CT scan is much more sensitive for thoracic injuries than is chest X-ray, the CT does not usually add clinical information that changes management. There are often very small pneumothoraces or contusions picked up incidentally, which require only observation. The exception to this is the mediastinal hematoma, which
may be a marker for underlying aortic injury.
Preparation of Patient
- Patients should have BUN/creatinine checked prior to intravenous contrast if there is risk of renal insufficiency.
- The oral hypoglycemic metformin may cause lactic acidosis when renal failure is present.
- Therefore, it should be held for 48 h after a contrast CT scan in case renal failure develops.
- No oral contrast is necessary for chest CT.
- Generally any patient undergoing chest CT for either traumatic or non-traumatic conditions will require ACLS-capable escort to CT.
Specific Conditions
Acute Aortic Disruption
- This condition is fatal in the majority of patients, who will die on scene of trauma.
The patients that survive are usually harboring a silent but fatal condition requiring a high index of suspicion. As will be discussed, plain radiography and even CT scan are used as screening tests instead of more invasive diagnostics such as aortography.
- Diagnosis of aortic disruption starts with suspicion of the injury, usually because of mechanism of injury, associated injuries or chest X-ray findings. Any high-speed acceleration or deceleration injury or fall leads to the aortic tear, which is at the root of this injury. The tear is most often at the descending aorta just past the left subclavian artery. The aorta is fixed at this level by the ligamentum arteriosum.
- Injury patterns seen in association with aortic disruption include flail chest, first rib fractures, sternal fracture or pelvic ring disruption. Chest X-ray findings are numerous and are covered elsewhere in this handbook.
- CT scan serves as a screening tool for mediastinal hematoma in the diagnosis of traumatic aortic disruption. The mediastinal hematoma is rarely from an aortic tear itself, but more often from small mediastinal vessels. If no hematoma is visualized, then no aortography is necessary. Mediastinal hematoma requires either CT aortography or
conventional aortography to rule out aortic injury.
Pitfalls in Aortic Disruption
- Failure to consider the diagnosis. Any patient with high-risk mechanism or symptoms/signs should undergo evaluation for aortic disruption.
- Failure to order CT scans in the presence of a normal mediastinum on chest X-ray.
Aortic disruption or its precursor, aortic intimal flap is well described with normal appearance on chest X-ray.
Non-Trauma
Aortic Dissection
- Aortic dissection is another potential disastrous condition that is often delayed in diagnosis due to variable presentation. The prognosis is good with early diagnosis and treatment.
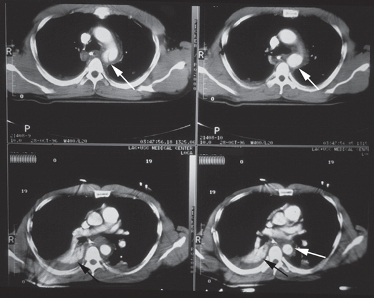
Figure: These four images reveal an aortic disruption. The white arrows reveal the intimal tear and surrounding mediastinal hematoma. The black arrows reveal an associated hemothorax.
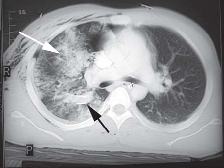
Figure: Pulmonary contusion. White arrow shows the pulmonary contusion. The black arrow outlines a chest tube previously inserted for a pneumothorax.
- The pathogenesis of aortic dissection begins with an intimal tear which will eventually dissect and in its worst form will either rupture proximally into the pericardium or rupture the surrounding adventia into the thorax, resulting in death.
- Aortic dissection is generally classified as either Stanford type A arising in the proximal aorta or Stanford type B arising in the aorta distal to the ligamentum arteriosum.
- Risk factors for dissection include hypertension, smoking, atheroscelerotic disease, collagen disorders and pregnancy.
- Clinical presentation is quite variable depending on site of dissection or occlusion of vessels. Pain, either located in the chest or back is present in almost all cases. The clinical presentation is covered in more detail elsewhere in the manual.
- There are many imaging options for aortic dissection, each with particular strengths or weaknesses:
- CT scan: CT aortography is a sensitive and specific test (80-100% and 90-100% respectively) for aortic dissection and is readily available in most facilities on a 24 h basis. It is noninvasive and may be performed quickly. It has replaced aortography for the initial evaluation of aortic dissection in most facilities.
- Disadvantages of CT scan include:
- Need for intravenous contrast dye.
- Inability to identify small intimal flap.
- Inability to identify involvement of the coronary arteries.
- Aortography: CT scan has almost replaced invasive conventional aortography as the primary method of investigating aortic dissection. Aortography may still have a role in questionable CT results or if detail is necessary regarding location of intimal flap or coronary artery involvement. It has a sensitivity close to that reported for CT scan.
- Disadvantages of aortography include:
- Invasive test.
- May not visualize dissection in the setting of thrombus in the false lumen.
- Not readily available, and angiography teams often take 1-2 h to assemble even under best circumstances.
Large intravenous contrast dye load.
- MRI: Magnetic resonance imaging is covered elsewhere in this handbook; however it deserves mention as a very sensitive test for aortic dissection with sensitivities reported as 100%. It has a number of key disadvantages that limit clinical use.

Figure: Aortic dissection is seen in the proximal ascending and descending aorta.
The white arrows identify the intimal tear.
- Disadvantages of MRI include:
- Lack of availability.
- The MRI scan is time-consuming, and proper monitoring of these critical patients is difficult.
- Transesophageal ultrasound (TEE): TEE is an excellent diagnostic tool for evaluating aortic dissection. It may be performed at the bedside, making it an excellent choice for unstable patients. It has excellent sensitivity (100%) and specificity and requires no intravenous contrast. It provides detail of the pericardium and the aorta
as well as the coronary arteries. As availability becomes more widespread, we may see its role increased.
- Disadvantages of TEE include:
- Minimally invasive.
- Availability, especially on a 24 h basis.
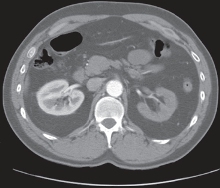
Figure: This image from the same patient shows a non-enhancing left kidney due to renal artery occlusion from the dissection.

Figure: This CT image of the descending aorta shows the intimal flap of the dissection in the mid-lumen.
Pulmonary Embolus
Advances in helical CT scanning have allowed CT to become quickly incorporated into the algorithm of evaluation of pulmonary embolus. While details of its role are being resolved in clinical trials, there is no doubt it will be a major tool in the diagnosis of pulmonary embolus.
Current evaluation of pulmonary embolus depends heavily on Bayesian algorithms involving indirect testing for PE. The history is paramount in the primary investigation of pulmonary embolus as it will determine the pre-test probability of all other diagnostics to follow. Traditionally, suspected pulmonary embolus is investigated using ventilation-perfusion nuclear scanning utilizing labeled radioisotopes to assess pulmonary arterial perfusion defects, indirect evidence of pulmonary embolism. Duplex ultrasound of the deep veins of the legs may also be used to search for venous thrombosis, which would also require anticoagulation and hopefully obviate the need for further investigation for pulmonary embolus. V-Q scanning is very sensitive and therefore a normal scan will give a negative predictive value of 100%, ruling out the disease. A high probability scan as determined by criteria
involving visualized perfusion defects not matched with ventilation defects, indicates presence of pulmonary embolus in over 90% of patients with high clinical suspicion of pulmonary embolus. A low probability V-Q scan in combination with low clinical suspicion yields <5% incidence of pulmonary embolus.
The problem in evaluating suspected pulmonary embolus patients comes with any combination of clinical suspicion and scans results other than low/ low or high/ high. This is the indeterminate gray zone, comprising the majority of patients. Traditionally pulmonary angiography is used to rule out pulmonary embolus; however most patients do not undergo this test and may either be anticoagulated inappropriately or not treated for their pulmonary embolus. Spiral CT scanning of the chest may help decrease the need for angiography.
Helical, or spiral CT scanning as it is termed, is a recent advance in CT technology whereby the patient is moved through the CT beam as it circles the patient thereby cutting scan time to 20 seconds with newer generation scanners. The patient will ideally hold her breath during the scan and scan cuts are usually 2 mm in width for pulmonary embolus evaluation. Patients receive intravenous contrast bolus at the time of scanning to provide adequate visualization of the pulmonary vasculature. Sensitivities in trials have been reported in a range of 50-100% but usually with high specificities. The origin of such variability is probably with difference in
scan techniques or whether subsegmental pulmonary emboli were considered.
Inherent Advantages of Helical CT Scanning
- Direct visualization of the embolus rather than indirect evidence of pulmonary embolus as with perfusion scanning.
- It may suggest an alternative diagnosis that may change treatment plan, i.e., you may not want to anticoagulate the patient with aortic dissection.
- Fast and readily available, usually on a 24 h basis.
- Highest inter-observer reliability when compared with V-Q scan or angiography.
Disadvantages of Helical CT Scanning
- May miss small subsegmental pulmonary emboli.
- Large intravenous contrast load.
- Breath-holding and contrast variation may affect results of scan.
- Negative predictive value has not yet been adequately established but will probably not match a normal perfusion scan.

Figure: This large saddle embolus causes filling defects bilaterally as shown by the white arrows.

Figure: This view from the same patient also reveals the large filling defect occluding the left main pulmonary artery (white arrow).
Today’s role of helical CT in evaluation of suspected pulmonary embolus is primarily in those patients with significant cardiopulmonary disease or abnormal chest X-ray, as these groups are most likely to have an indeterminate perfusion scan.
|